Emerging Applications of Microwave Energy in Medical Research
The science of microwave energy is being widely explored, and several conditions are under active early-stage investigation. These investigations are focused on understanding its effects and potential applications across various fields.
Interested in the possibililities
of Microwave Energy? Submit a Medical Device Information Request
The following conditions represent just a few of those currently of interest from a scientific research perspective
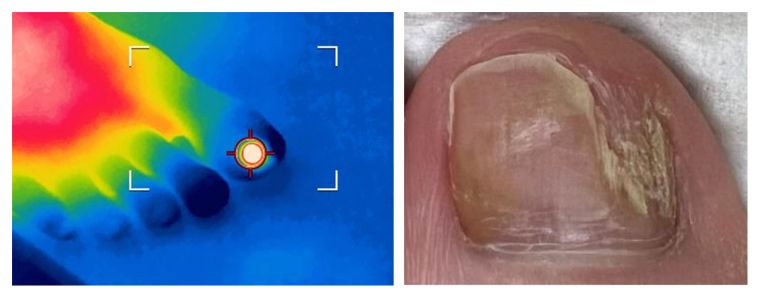
Clinical Summary of Onychomycosis:
Onychomycosis is a common fungal infection of the nails, characterised by thickened, brittle, discoloured, and deformed nails, most commonly affecting the toenails. The condition is caused by dermatophytes, non-dermatophyte moulds, or yeasts, such as Trichophyton rubrum or Candida species, which invade the nail plate and surrounding tissue. Risk factors include advancing age, diabetes, immunosuppression, poor peripheral circulation, and environmental exposure to moist conditions, such as public swimming pools or communal showers. Onychomycosis can significantly impact quality of life due to pain, cosmetic concerns, and the potential for secondary bacterial infections.
Prevalence:
Onychomycosis is the most common nail disorder, accounting for 50% of all nail diseases. Its prevalence is estimated to be 10-20% globally, with higher rates observed in adults and older populations. The condition is more common in males than females and occurs more frequently in individuals with underlying conditions such as diabetes or peripheral vascular disease. Prevalence is rising worldwide, driven by ageing populations and increasing rates of chronic illnesses that predispose individuals to fungal infections.

Clinical Summary
Neurovascular corns, also known as Intractable Plantar Keratosis (IPK), are painful, thickened lesions that develop on the soles of the feet, typically in areas exposed to chronic pressure or friction. These lesions are characterized by the involvement of both nerve and blood vessels, making them particularly painful and difficult to treat. They often present as well-defined, callous-like growths with a deep central core, causing significant discomfort during weight-bearing activities. Recent reports in the literature have identified co-infection with human papillomavirus (HPV) in neurovascular corns, detected through PCR analysis. This viral presence may contribute to the persistence and treatment resistance of these lesions.

Clinical Summary and Prevalence
Molluscum contagiosum is a viral cutaneous infection caused by Molluscum contagiosum virus (MCV), a poxvirus, characterized by firm, umbilicated papules that commonly occur on the skin and mucous membranes. Transmission occurs via direct skin contact, autoinoculation, or fomites, with sexual transmission being common in adults.
Prevalence: The infection is most prevalent in children (5-10%) and immunocompromised individuals, such as those with HIV.

Clinical Summary and Prevalence
Hidradenitis suppurativa (HS) is a chronic, inflammatory skin condition characterized by the development of painful nodules, abscesses, and tunnels (sinus tracts) in areas where skin rubs together, such as the armpits, groin, buttocks, and under the breasts. The condition often starts with small, tender bumps that can progress to abscesses, which may rupture and form scarring and deep tunnels over time. While the exact cause of HS is not fully understood, it is thought to involve a combination of follicular occlusion, hormonal influences, genetic predisposition, and immune dysregulation. HS can severely impact quality of life due to persistent pain, scarring, odor, and recurrent flare-ups, often leading to social and psychological distress.
Prevalence (HS) is estimated to be between 1-4% of the global population, though it may be underreported due to misdiagnosis or delayed diagnosis. HS tends to be more common in females, with a female-to-male ratio of about 3:1. It typically begins after puberty, with peak incidence occurring in individuals aged 20-40 years. Additionally, there is a higher prevalence of HS among individuals with certain risk factors, including obesity, smoking, and a family history of the condition.

Clinical Summary and Prevalence
Cystic acne is a severe form of acne vulgaris characterized by deep, inflamed, and often painful nodules or cysts that develop due to obstruction and rupture of the sebaceous glands with subsequent inflammation. The condition is typically driven by hormonal changes that increase sebum production, keratinocyte proliferation, and Propionibacterium acnes colonization. It most commonly affects the face, chest, and back and can lead to scarring if untreated.
Prevalence: Cystic acne primarily affects adolescents and young adults, with a higher incidence in males during adolescence due to androgenic stimulation. It occurs in approximately 20-30% of individuals with acne, but its exact prevalence varies globally. Severe cases are less common, but untreated cystic acne may persist into adulthood.

Clinical Summary of Solar Lentigo:
Solar lentigines, also known as age spots, liver spots, or sunspots, are benign, hyperpigmented lesions that appear on sun-exposed areas of the skin, such as the face, hands, shoulders, and arms. They are caused by prolonged exposure to ultraviolet (UV) radiation, which stimulates melanocyte activity and results in localised melanin accumulation. These lesions are typically flat, well-defined, and vary in size and colour, ranging from light brown to dark brown. Solar lentigines are primarily a cosmetic concern and are not pre-cancerous; however, their presence signifies significant UV exposure, which is a known risk factor for skin cancer.
Prevalence:
Solar lentigines are highly prevalent, particularly in older adults, with their incidence increasing with age and cumulative UV exposure. They are most commonly seen in individuals over the age of 40 and are more frequent in fair-skinned populations. Studies estimate that up to 90% of people over 60 have at least one solar lentigo. Their prevalence is higher in regions with intense sunlight and among those with outdoor lifestyles, emphasising the importance of sun protection for prevention.

Clinical Summary and Prevalence
Squamous Cell Carcinoma in Situ (SCCis), also known as Bowen's disease, is an early, non-invasive form of squamous cell carcinoma confined to the outermost layer of the skin (the epidermis). It typically presents as a persistent, scaly, red, and sometimes crusted patch on sun-exposed areas such as the face, neck, hands, and legs, but can also appear on mucous membranes. Lesions may be slightly raised, have irregular borders, and can grow slowly over time. While not immediately life-threatening, SCCis has the potential to progress to invasive squamous cell carcinoma if left untreated, which can then penetrate deeper skin layers and metastasize. Risk factors include prolonged UV exposure, fair skin, older age, immunosuppression, and a history of chronic skin injuries or human papillomavirus (HPV) infection.
Prevalence: SCCis is a relatively common precancerous skin condition, particularly in fair-skinned individuals over 60 years of age. It is more frequently diagnosed in women than in men and occurs more often in areas with high UV exposure, such as Australia, New Zealand, and parts of North America and Europe. The exact prevalence is difficult to determine, but its incidence has been on the rise due to increased UV exposure from outdoor activities, tanning bed use, and an aging population. SCCis represents an early stage of squamous cell carcinoma, and prompt diagnosis and treatment can significantly reduce the risk of progression to invasive cancer.

Clinical Summary and Prevalence
Basal cell carcinoma (BCC) is the most common form of skin cancer, arising from the basal cells in the epidermis. It typically presents as a slow-growing, locally invasive lesion, often appearing as a pearly, translucent nodule with telangiectasia or as a non-healing ulcer, particularly on sun-exposed areas of the skin such as the face, neck, and arms. Chronic ultraviolet (UV) exposure is the primary risk factor, along with fair skin, advanced age, and a history of sunburn.
Prevalence: BCC accounts for approximately 75-80% of all skin cancers, with an estimated lifetime risk of 20-30% in Caucasians. The incidence is higher in fair-skinned individuals, those with a history of significant UV exposure, and older populations. It is less common in individuals with darker skin tones.

Clinical Summary and Prevalence
Melanoma is an aggressive form of skin cancer that originates in the melanocytes, the cells responsible for producing melanin, the pigment that gives skin its colour. It often presents as a new or changing mole, characterized by asymmetry, irregular borders, varying colours, large diameter (greater than 6 mm), and evolution over time (ABCDE criteria). While melanoma can occur on any skin surface, it most commonly appears on sun-exposed areas such as the back, legs, arms, and face. It can develop quickly and has a higher potential to spread (metastasize) to other parts of the body, including the lymph nodes, lungs, liver, and brain, making early detection and treatment crucial for improving survival rates. Major risk factors include excessive UV exposure, fair skin, a history of sunburns, numerous moles, a family history of melanoma, and genetic predispositions.
Prevalence: Melanoma is less common than other types of skin cancer, but it is the most serious due to its high potential for metastasis. Worldwide, the incidence of melanoma has been rising, with an estimated 325,000 new cases diagnosed annually. In regions like Australia and New Zealand, rates are among the highest, likely due to high UV exposure and a predominantly fair-skinned population. In the United States, the lifetime risk of developing melanoma is about 1 in 38 for whites, 1 in 1,000 for African Americans, and 1 in 167 for Hispanics. Although it can occur at any age, melanoma is most frequently diagnosed in older adults, though it is also one of the most common cancers in young adults, particularly women under 30.
 UK & Ireland
UK & Ireland  Deutschland
Deutschland  United States
United States